Beyond Adherence
Redesigning Apple Health to help patients manage and predict the triggers and symptoms of chronic disease.
Disclaimer:
This is a self-initiated research project exploring opportunities to enhance Apple Health's medication tracking functionality. This work is not affiliated with, or endorsed by, Apple Inc. The concepts, designs, and recommendations presented are speculative and intended to demonstrate design thinking, research methodology, and problem-solving capabilities. Patient scenarios are fictional and developed for illustrative purposes to test hypotheses about user needs and potential solutions.
TL;DR
I redesigned elements of Apple Health's medication tracker to transform it from a basic adherence tool into a comprehensive chronic disease management platform.
Through research-driven design, I evolved the concept from simple medication logging to integrated symptom tracking, and ultimately to predictive health intelligence powered by multi-source data integration.
The Problem: Apple's current medication tracker treats adherence as a binary "taken/not taken" function and misses the opportunity to help patients with chronic conditions understand symptom patterns, identify triggers, and develop proactive management strategies.
The Solution: A three-phase enhancement that enables symptom logging alongside medication tracking, adds trigger identification capabilities, and ultimately integrates data from across the Apple Health and software ecosystem (sleep, nutrition, activity, hormonal cycles, location data, calendar) to provide insights that help patients manage their health.
The Impact: For patients like Emma, a fictional character I developed using Claude to test my hypothesis, this approach transforms reactive symptom treatment into proactive health management and the potential to reduce medication dependency and improve quality of life through better symptom prediction and prevention.
This project demonstrates how user-centred design, combined with a deep understanding of chronic disease, can challenge the capabilities of emerging health technology and transform existing products into genuinely transformative health tools.
This work is important to me because…
Living with a chronic health condition, I know first-hand that most health tech is inadequate for people managing complex chronic conditions. I've tracked symptoms manually for years to try to identify patterns and better understand my body.
From developing FebriSol, I learned the power of human-centred design in healthcare. This work enabled me to explore its potential in digital health tools.
This project merges personal experience with professional practice. Every insight about symptom prediction comes from the lived experience of managing an unpredictable condition. It represents my belief that good design should empower people, not just digitise processes.
This work is important to you because…
Strategic product thinking: Three-phase approach balances immediate value with long-term vision, showing how to evolve existing platforms incrementally.
Real impact potential: Patient scenarios demonstrate how design decisions affect daily life, showing a genuine understanding of chronic disease management.
Cross-disciplinary collaboration: Bridges design, healthcare, and technology with domain expertise valuable for health tech companies.
Technical feasibility awareness: Progression from manual tracking to AI predictions demonstrates understanding of current capabilities and future possibilities.
Long Form Case Study
Context
We live in an era of remarkable medical advancement, with effective treatments available for countless chronic conditions. Yet the best medication in the world remains worthless if patients don't take it as prescribed. This fundamental challenge affects millions: adherence rates hover between just 60-70%, even in optimistic estimates.
Apple's 2022 integration of medication tracking within the Health app represents a significant step forward. Previously, chronic patients relied on workarounds like the Reminders app and other tools never designed for the complexities of chronic disease management. Apple's solution offers proper medication logging, 'as needed' tracking, and visual progress monitoring.
“On average across 24 OECD countries, more than one-third of adults reported living with a longstanding illness or health problem in 2021” [SRC], an indicator that a more comprehensive and integrative approach to adherence and chronic disease management would likely be relevant to Apple’s users.
For tech-savvy users managing straightforward regimens, Apple’s medication tracker works reasonably well. But something is missing; the current tracking tool focuses purely on adherence, treating medication management as binary: taken or not taken. This approach overlooks the rich, interconnected data Apple Health collects, which could transform how patients understand and manage their conditions.
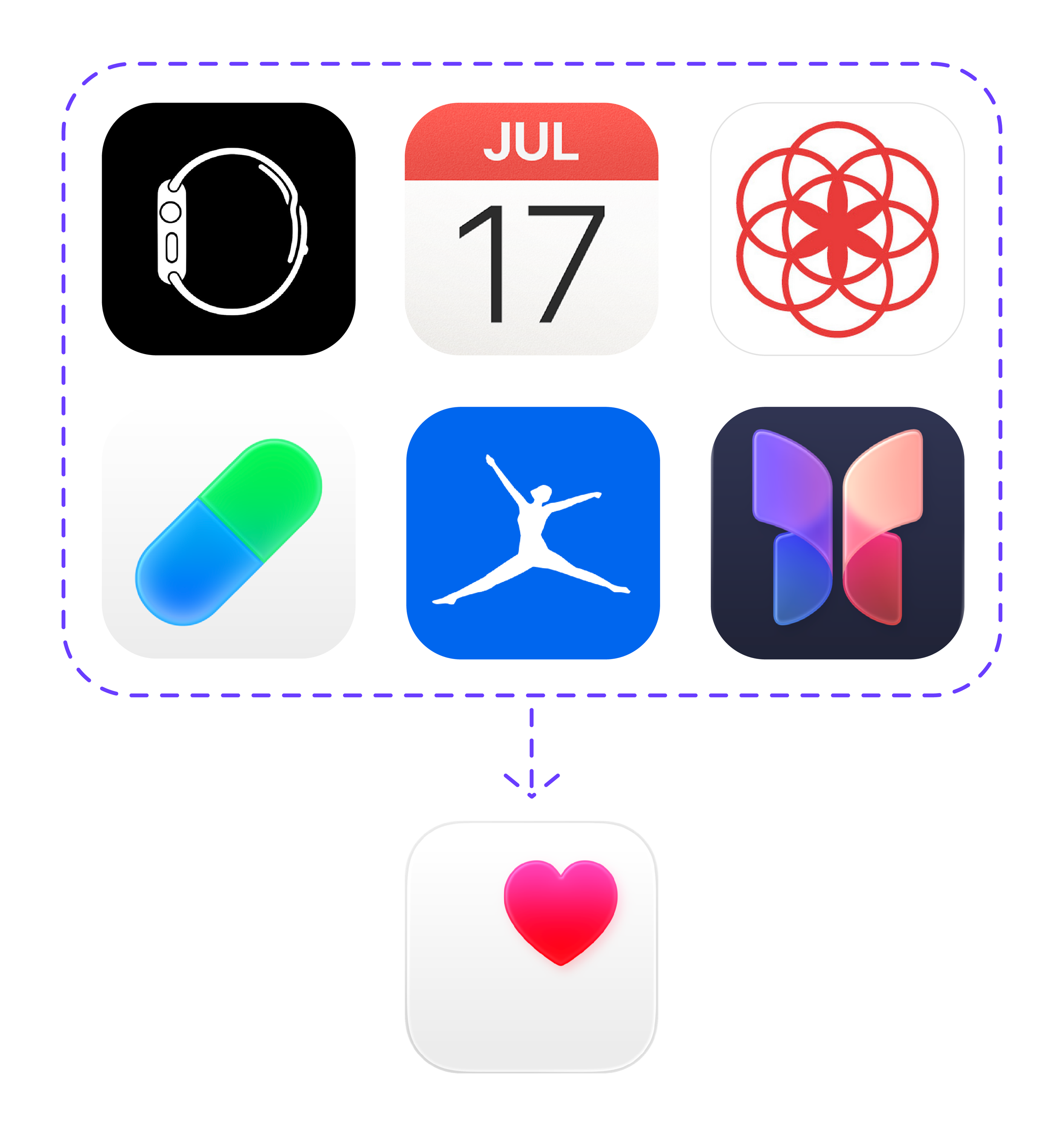
Apple Health sits uniquely positioned in the digital health ecosystem. Unlike competitors such as Oura or Whoop that focus on single data streams, Apple Health acts as a centralised hub, pulling information from multiple sources: activity trackers including Apple Watch, Oura and Whoop, nutrition apps like MyFitnessPal, blood testing services like Thriva, and now medication tracking.
However, whilst Apple excels at data collection and presentation, it avoids making inferences or connections between data points.
This design philosophy works well for fitness tracking but falls short for chronic disease management, where understanding relationships between symptoms, medication use, environmental factors, and lifestyle choices can be transformative for patient outcomes.
Problem Statement
Can Apple Health's medication tracker become a tool that empowers patients with chronic conditions to identify patterns, understand triggers, and develop healthier long-term behaviours through integrated symptom tracking and data insights?
Research
Academic research consistently demonstrates that self-tracking becomes most powerful when it extends beyond data collection toward pattern recognition and behaviour change.
Studies across chronic disease management show that systematic tracking helps patients improve their knowledge about the illness, identify triggers, pain management and control health indicators such as glucose levels or blood pressure [SRC].
The evidence base for symptom tracking in chronic disease management is substantial. Research focusing on chronic illness management demonstrates effectiveness across diverse conditions, including cancer, autoimmune conditions, heart disease, irritable bowel syndrome, and asthma.
These studies generally aim to ‘control or mitigate symptoms and to prevent or delay disease progression’ through systematic data collection.
-
RTHM, a California-based health tech specialising in remote monitoring and chronic disease management, recognises a fundamental challenge: "When there aren't accessible blood tests to monitor treatment success, how do you know what treatments are working?" [SRC]
They argue that systematic symptom and activity tracking provides patients and healthcare providers with "a comprehensive picture of current health challenges, assists clinicians in making diagnoses, and helps understand what treatments are working."
Their approach offers several critical advantages:
Disease progression monitoring: Tracking symptoms over time provides insights into condition progression, helping patients and providers understand whether symptoms are improving or worsening.
Treatment efficacy assessment: Patients can see firsthand what treatments provide relief, helping them "regain some of their power" in managing their condition.
Pattern identification: Systematic tracking allows patients to identify trends and understand their personal health patterns.
-
As a chronic pain patient, I've experienced both the potential and limitations of current tracking approaches.
Manual tracking in paper diaries captures rich contextual information about triggers and symptoms, but makes pattern identification nearly impossible. I meticulously log medication intake to track trends, identify causal links, and ensure I'm not developing dependency, but the manual nature of the process creates significant barriers.
Digital tools like Apple's tracker are excellent at data collection but fail to surface the connections that matter most to patients like me. The current system allows me to see graphs showing medication compliance, but I cannot easily identify why certain days require more 'as-needed' medication or how external factors influence my condition.
-
Research into self-tracking engagement patterns provides crucial insights for design. Studies show that "the probability of routine self-tracking is higher for those who use technological tools" and that "the use of technological tools such as websites and tracking apps facilitates this practice." Conversely, when patients "rely on memory to do self-tracking, the chance that they will collect data routinely is significantly decreased" [SRC].
The shift towards mobile health solutions has accelerated, particularly following COVID-19. Mobile applications have "matured and become increasingly used in chronic disease management for patient education, monitoring, and interactions," showing "positive trends in patient adherence to chronic disease management." These tools prove effective in "reducing hospital burden, obtaining reliable information, tracking symptoms, and improving mental health" [SRC].
-
The barrier to meaningful insights remains frustratingly high. Current tools represent a fundamental design flaw: building what designers think patients need rather than what patients actually require.
Effective symptom tracking systems should include symptom description, frequency and duration, activity level, sleep patterns, emotional well-being, environmental factors, and physiological measures to "create a comprehensive picture of health over time" [SRC].
The opportunity lies in creating feedback loops that turn raw tracking data into personalised health management. Research demonstrates that effective systems can identify patterns that would otherwise remain hidden, providing "the temporal resolution needed to detect indicators of future relapse or remission in long-term conditions" [SRC].
This capability would enable patients to move from simply recording what happened to understanding why it happened and how to prevent it from recurring, transforming Apple Health from a data repository into a genuine health management partner.
Manual Tracking:
Ideation, Design & Testing



Disclaimer:
The following patient scenario featuring ‘Emma’ and her management of Ehlers-Danlos Syndrome was developed as a hypothetical case study using a combination of Claude AI and my personal experience with chronic condition management.
This scenario is designed to demonstrate and test hypotheses about user needs, behaviour patterns, and potential solutions in chronic disease management. While grounded in research and real-world insights, Emma’s specific symptoms, medication regimen, and tracking outcomes are illustrative examples created for research and design exploration purposes and should not be considered medical advice or indicative of all patients managing a chronic condition.
This is Emma…
Background:
Emma is 28 years old and lives with Ehlers-Danlos Syndrome (EDS) a chronic condition affecting her connective tissue, caused by defects in collagen production. EDS affects the skin, joints, and blood vessels.
The condition is characterised by joint hyper-mobility leading to frequent dislocations, chronic pain, fragile, stretchy skin that bruises easily, and often severe fatigue. Patients with EDS typically experience unpredictable symptom flares, generalised anxiety, brain fog, muscle spasms, and may require various medications to manage pain, inflammation, and associated complications on an 'as needed' basis.
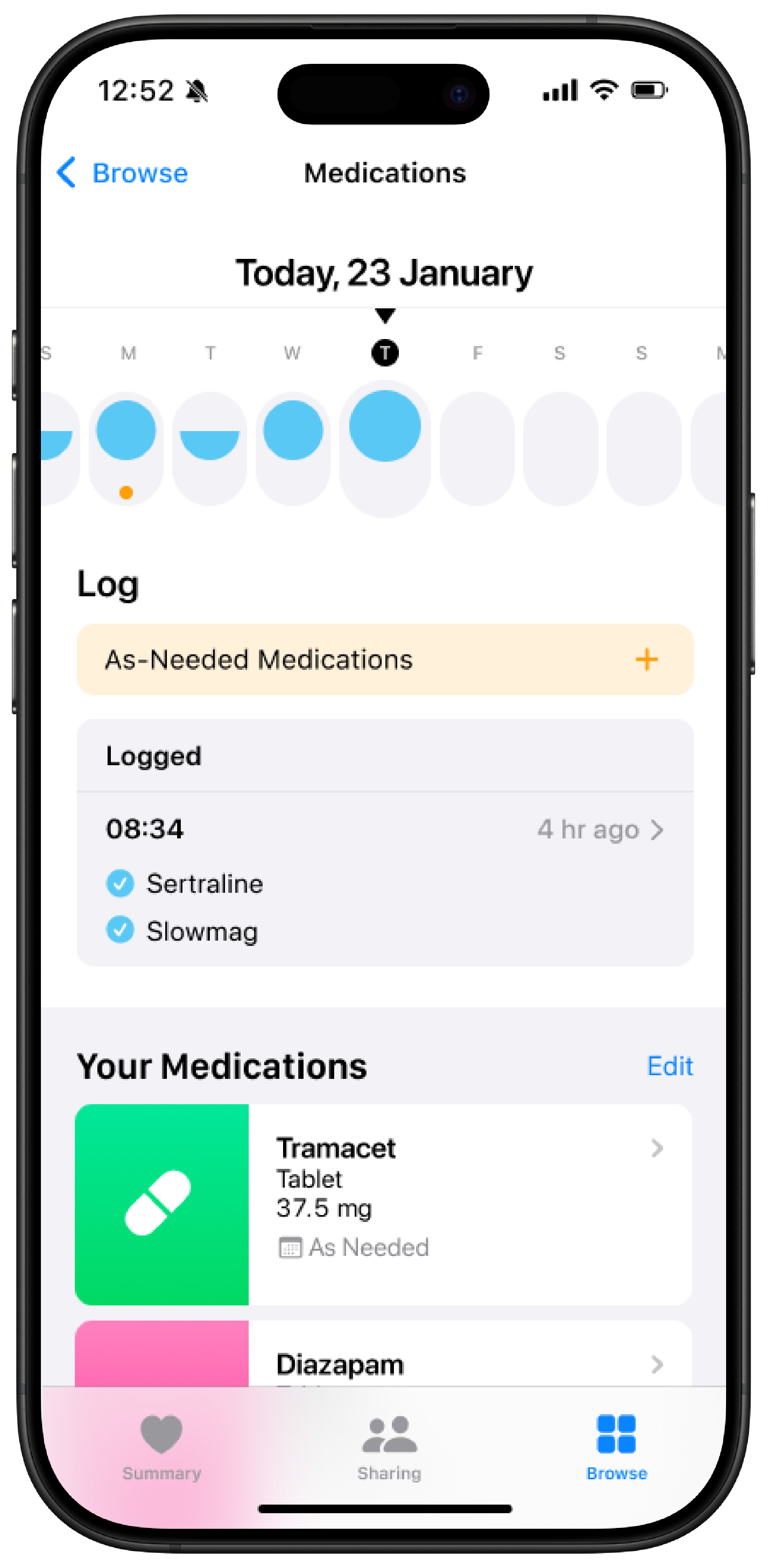
She takes daily SSRI for mood management and magnesium to prevent muscle spasms, alongside various 'as-needed' medications for symptomatic flare-ups.
Current Medication Regime:
Daily medications: SSRI (escitalopram), Magnesium
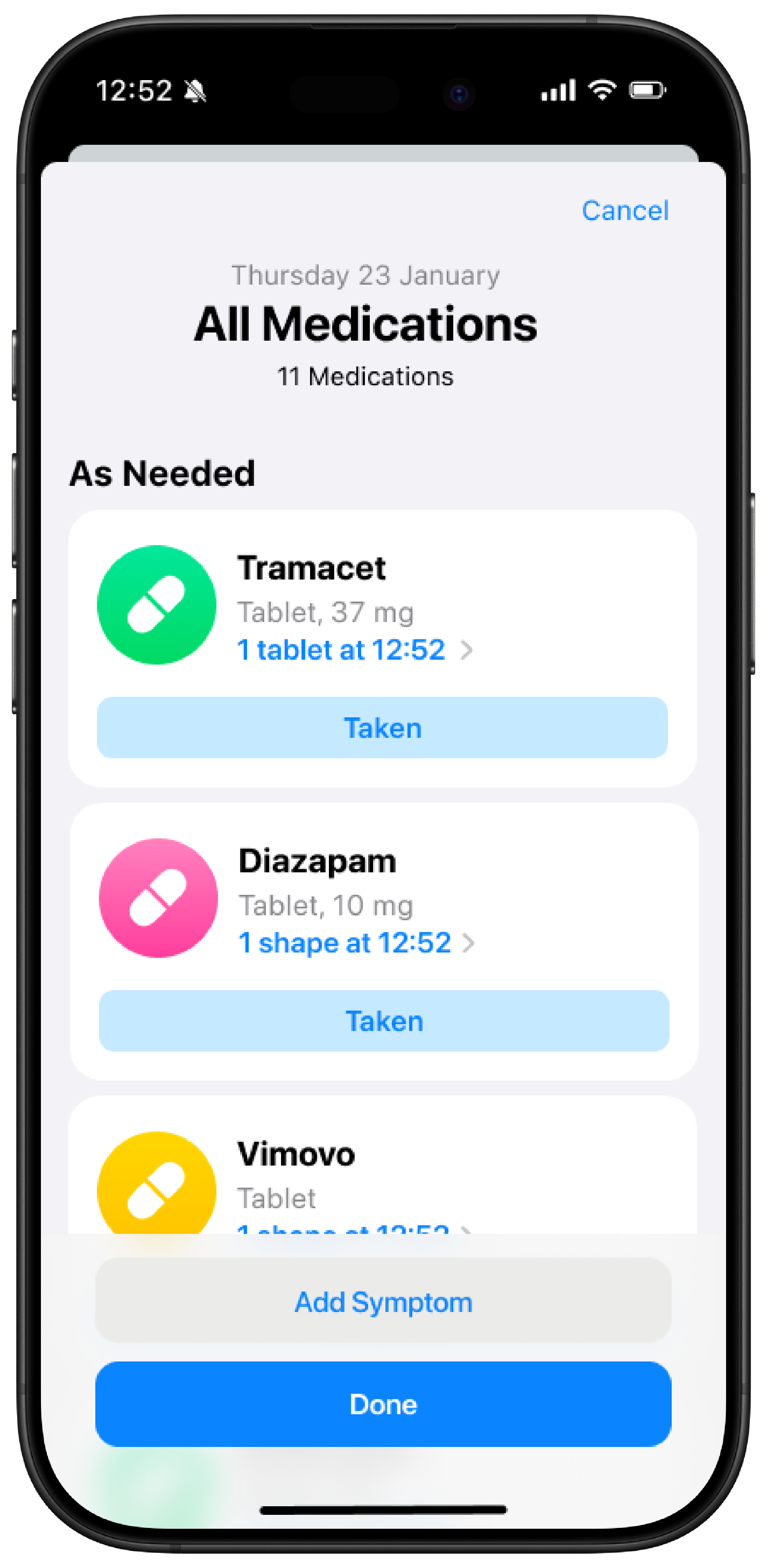
As-needed medications: Tramacet (pain), Vimovo (inflammation), Diazepam (muscle spasms), Ritalin (brain fog)
As/Is Screenshots:
Apple medication Home Screen. Adherence based on the binary: taken/not taken.
Ability to add ‘as-needed’ medication transforms a reminder into an adherence tool.
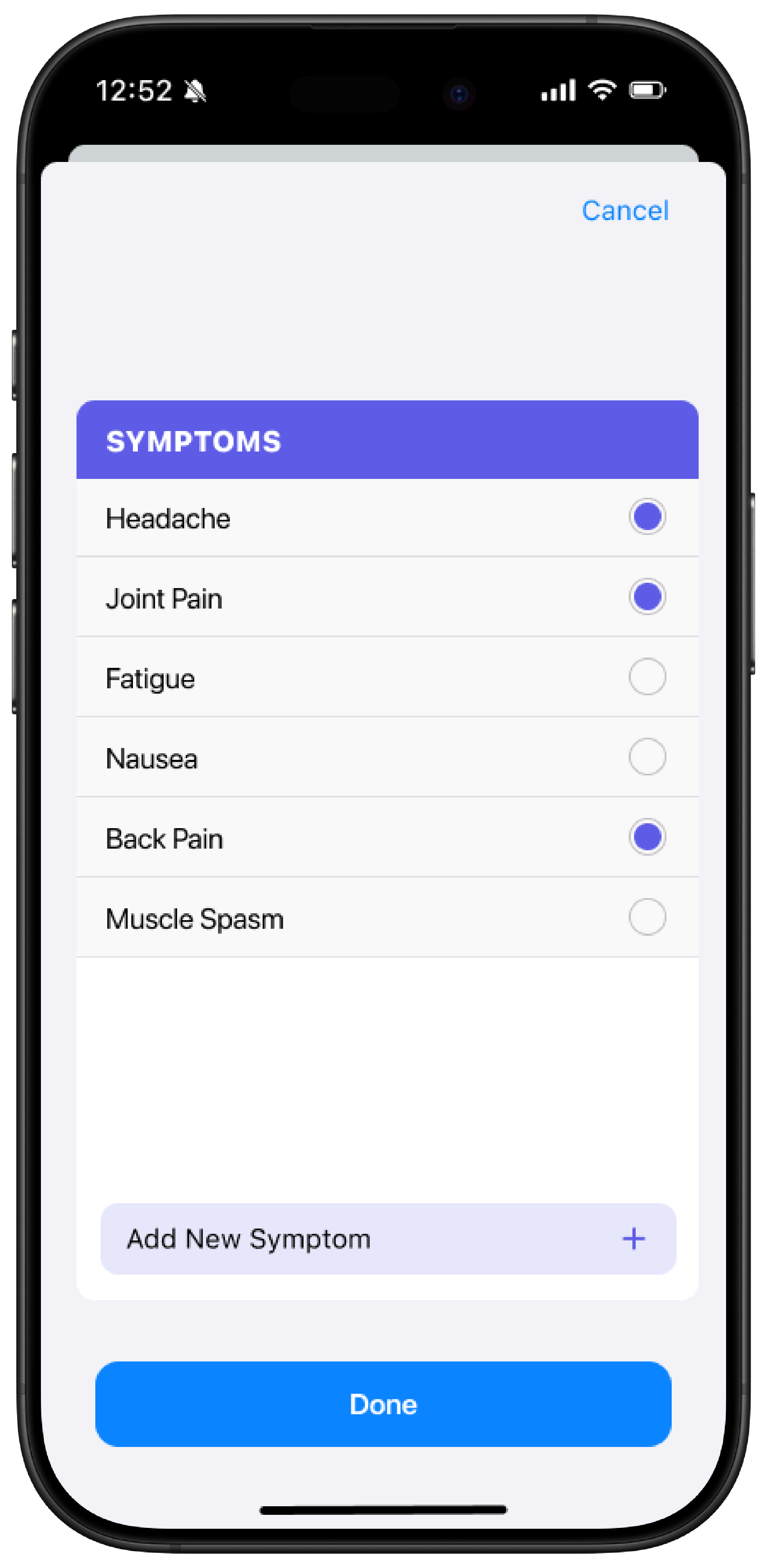
Cycle tracking feature of Apple Health enables user to log symptoms from a predetermined list.
Cycle tracking uses different ‘markers’ to differentiate between symptoms and menstruation.
V01: Basic Symptom Tracking
Enhanced Functionality:
Design based on Apple Cycle tracking
Log all medications (daily + as needed)
‘As-Needed’ marker indicated symptoms were likely present
Add symptoms: joint pain, headaches, back pain, bruising, swelling, fatigue, brain fog, muscle spasms, etc.
View frequency charts and symptom patterns
Design system for identifying whether chronic or as needed medication has been taken is based on Apple’s cycle tracking.
Functionality includes adding symptoms to logging as-needed medication.
Cycle tracking functions as the design system, with the added functionality to add customised symptoms.
Tagging symptoms enables the system to produce comprehensive reports of medication intake and symptomatic attacks.
Sarah's Experience After 6 Weeks:
Previously, Emma had no clear picture of her symptom patterns. She knew she had "bad days" and "good days" but couldn't quantify or predict them.
Key Insights from Tracking:
Frequency awareness: Emma discovers she experiences joint pain 18 days out of every month, far more than she realised.
Symptom clustering: The app shows that when she logs severe joint pain, she's 80% likely to also log fatigue the same day.
Medication patterns: She sees that she takes tramacet an average of 12 times per month, but the frequency varies dramatically (2-3 times some weeks, 6-7 times others).
Hidden symptoms: Back pain, which she barely noticed consciously, appears 15 days per month in her logs.
Behaviour Change: Emma starts taking her daily magnesium more consistently after seeing how muscle spasm frequency correlates with missed doses. She also begins to anticipate fatigue on high joint pain days, planning her work schedule accordingly.
V02: Trigger Integration
Enhanced Functionality:
All previous features, plus:
Add triggers: playing soccer, standing for long periods, work stress, menstrual cycle, lifting heavy objects
View correlations between triggers, symptoms, and medication use
Sarah's Experience After 8 Additional Weeks:
Powerful Trigger-Symptom Connections:
Physical Activity Revelation: Sarah discovers that playing soccer (which she does twice weekly) leads to severe joint pain within 24-48 hours 90% of the time. More surprisingly, the data shows she takes 3x more tramacer in the two days following soccer compared to her baseline.
Work Stress Cascade: The app reveals that high work stress days correlate with increased muscle spasms (requiring diazepam) and brain fog (requiring Ritalin) the following day. Sarah sees she takes 60% more 'as needed' medication the day after logging high stress.
Standing Pattern: Sarah tracks "standing for long periods" during design conferences and client meetings. The data shows that after standing for more than 3 hours, she experiences back pain 85% of the time and takes vimovo within 6 hours.
Real-World Behaviour Changes:
Soccer Strategy: Instead of giving up soccer entirely, Sarah plans around it. She ensures she has no major deadlines the two days following games, keeps tramacet readily available, and schedules lighter work activities for Tuesday and Thursday mornings.
Work Stress Management: Seeing the clear data connection between stress and next-day symptoms, Sarah starts using stress management techniques proactively. When she logs high stress, she takes magnesium that evening and prepares for potential brain fog the next day by scheduling less cognitively demanding tasks.
Event Preparation: Before conferences or long meetings, Sarah now takes vimovo preventatively and brings a portable seat, reducing her reactive medication use by 40% on these days.
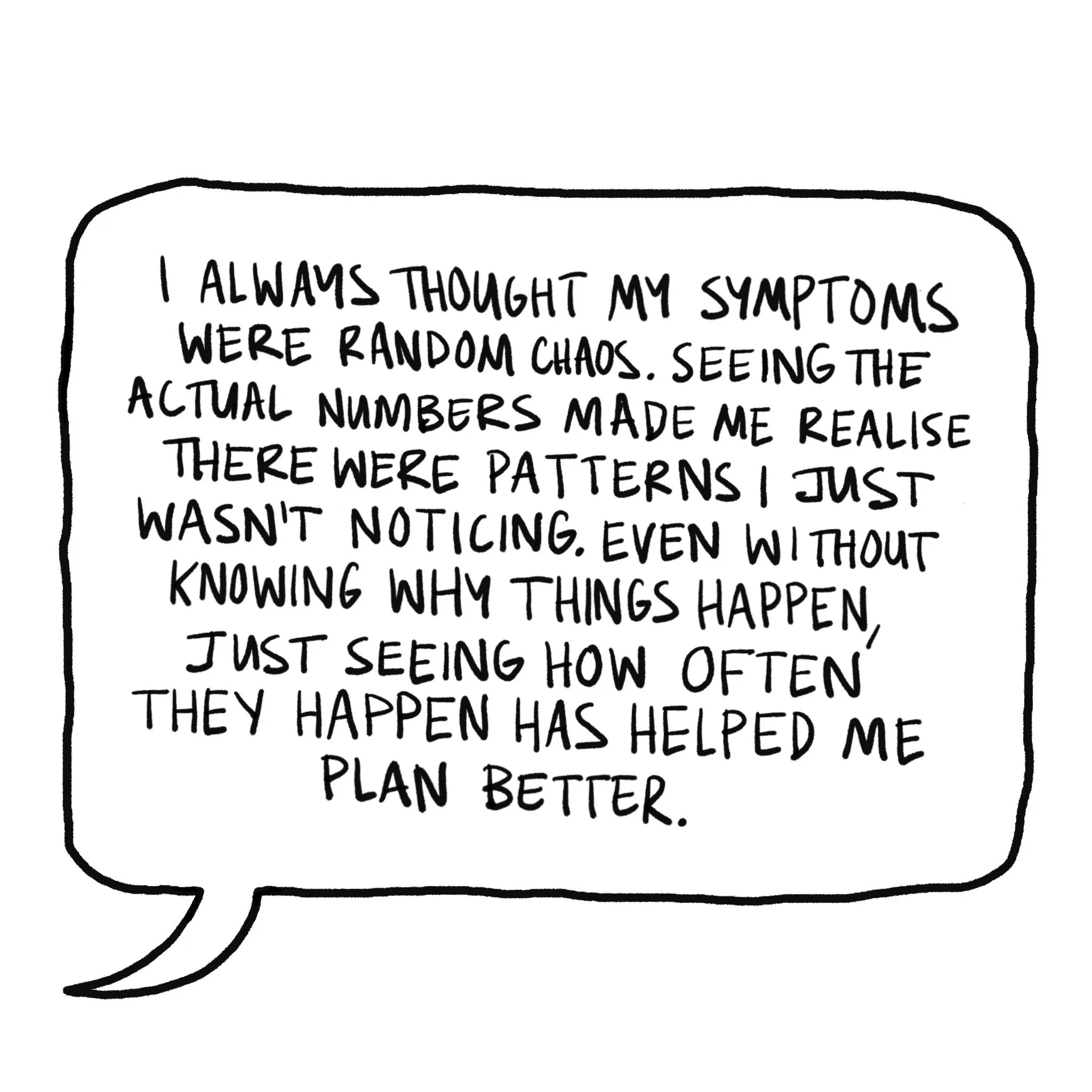
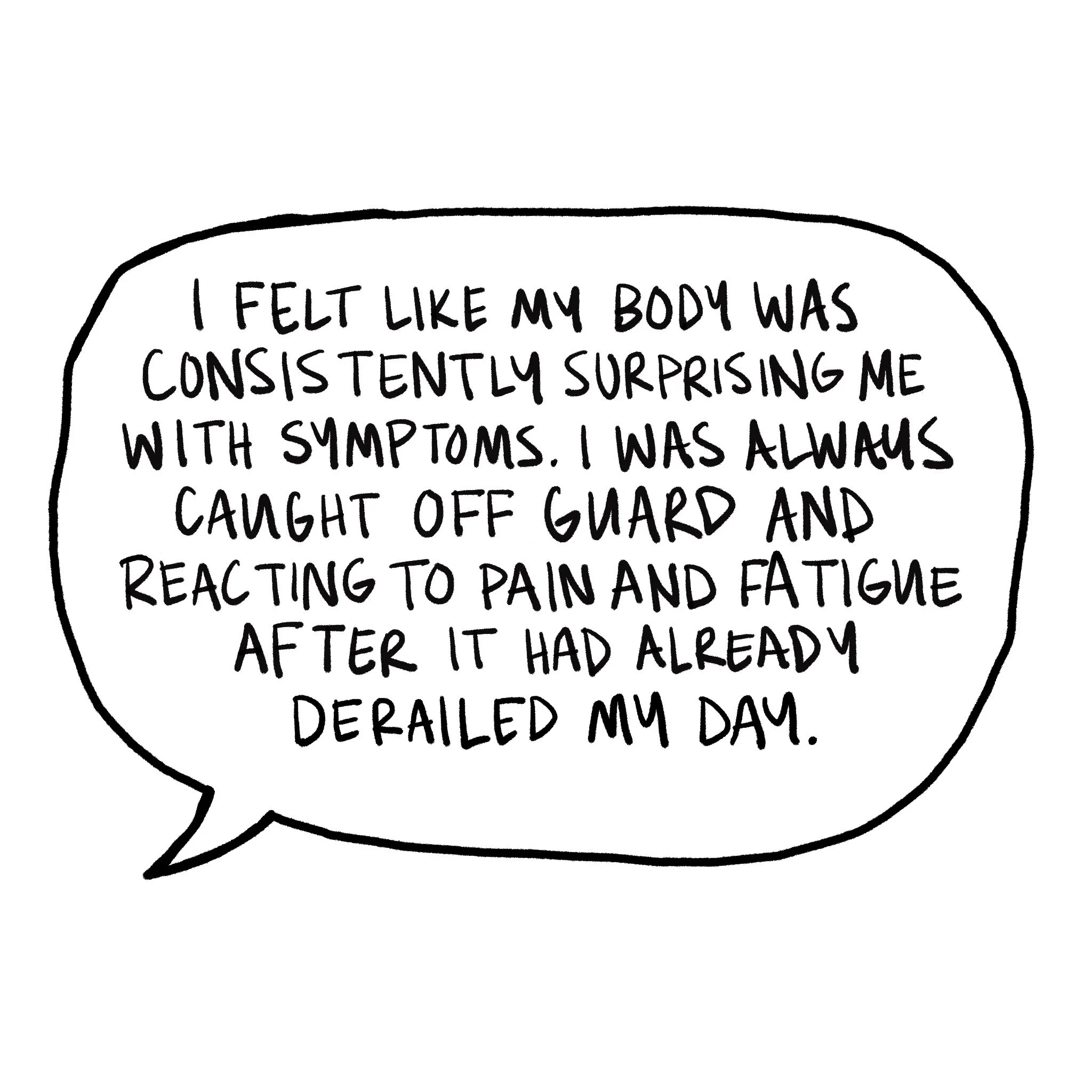
Before Tracking
After Enhanced Tracking
The Future Vision: Emma’s Fully Integrated EDS Management
Sarah's Connected Ecosystem:
Apple Watch: Sleep stages, heart rate variability, body temperature, O2 saturation, VO2 max, detailed activity tracking
Clue: Menstrual cycle phases, symptoms, mood tracking
MyFitnessPal: Nutrition intake, meal timing, hydration
Apple Health Journal: Daily reflections, mood, stress levels, energy ratings
Enhanced Medication Tracker: All previous symptom and medication logging
Calendar: Integrate daily activities and commitments
Time in Daylight: Vitamin D, mood management
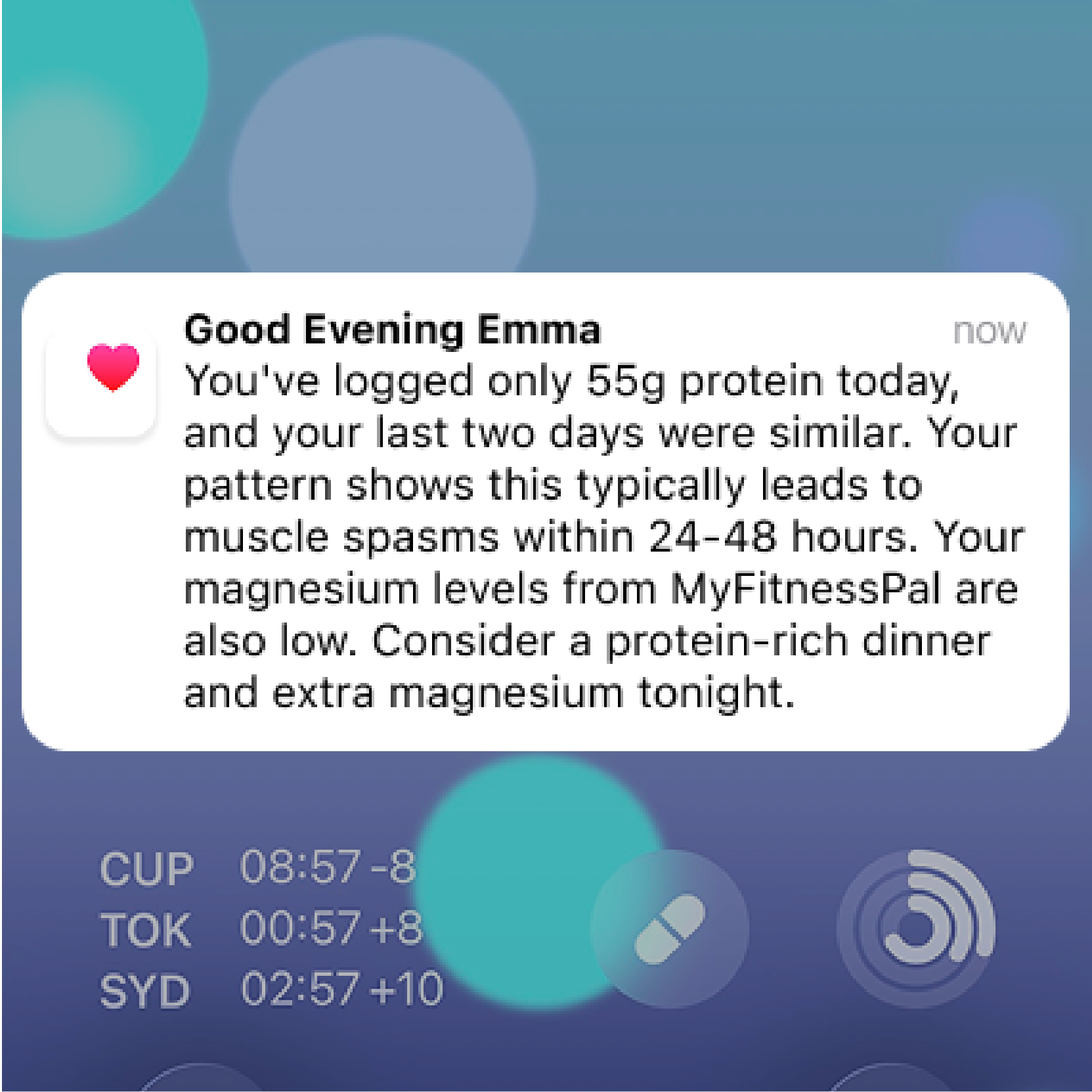
Predictive Intelligence in Action:
Nutrition Intervention
Activity Optimisation
Pre-Emptive Alert
Revelations from Integrated Data
Menstrual Cycle Discovery:
Sarah's manual tracking showed joint pain patterns, but the integrated data reveals something profound: her joint pain severity increases by 200% during the luteal phase of her cycle (days 15-28). More remarkably, the app correlates this with:
HRV drops: Heart rate variability decreases significantly 3-4 days before joint pain spikes
Sleep fragmentation: Deep sleep decreases by 30% during luteal phase
Medication timing: 70% of her codeine use occurs during days 20-28 of her cycle
Hidden Nutrition Connection:
Integration with MyFitnessPal uncovers unexpected patterns:
Protein correlation: Days with less than 80g protein correlate with increased muscle spasms and diazepam use 24-48 hours later
Hydration insight: Dehydration (less than 2L water) leads to increased headaches and fatigue, requiring more Ritalin
Iron deficiency pattern: Low iron days (tracked through nutrition) correlate with higher heart rate and increased fatigue symptoms
Sleep Quality Cascade:
Apple Watch sleep score reveals intricate connections Sarah never suspected:
REM sleep impact: Poor REM sleep (under 15% of total sleep) predicts brain fog severity with 85% accuracy
Deep sleep correlation: Less than 1 hour of deep sleep leads to increased joint pain and 3x higher anti-inflammatory use the next day
Sleep efficiency: When sleep efficiency drops below 80%, Sarah's HRV decreases and stress levels spike, leading to muscle tension requiring diazepam
Before Integration
After Integration
Pros & Cons of the Fully Integrated Health App
Pros
-
The integrated app moves beyond reactive symptom management to health intelligence.
By connecting Emma’s menstrual cycle data, sleep metrics, nutrition intake, and biometric trends, the app can predict EDS flares with 85% accuracy.
This enables proactive medication management, reducing her overall 'as needed' medication use by 50% whilst improving symptom control. The predictive capability transforms patients from feeling helplessly controlled by their condition to being empowered with advance warning and actionable insights.
-
The app identifies complex multi-factor relationships that would be impossible for patients or clinicians to spot manually.
Emma’s discovery that poor protein intake correlates with muscle spasms 48 hours later, or that HRV drops predict joint pain with high accuracy, represents the kind of sophisticated pattern recognition that can only emerge from analysing thousands of data points simultaneously.
This enables for personalised medication regimes based on individual physiological patterns rather than generic treatment protocols.
-
The integrated data transforms the patient-provider relationship by providing clinicians with rich, objective insights into how a patient's condition manifests in daily life.
Rather than relying on quarterly appointments and subjective symptom recall, healthcare providers can access comprehensive reports showing the interplay between physiology, lifestyle factors, and symptom patterns.
This enables more informed treatment decisions and truly collaborative care management.
Cons
-
The app requires access to deeply personal and sensitive health information across multiple platforms: menstrual cycles, mental health data, detailed sleep patterns, medication use, and daily mood reflections.
This creates a comprehensive digital health profile that, if breached or misused, could have devastating consequences for users.
The integration of data from multiple third-party apps (Clue, MyFitnessPal, Apple Health) creates multiple potential failure points and raises concerns about who has access to this information and how it might be used by employers, insurers, or other entities.
-
The sophisticated tracking system requires consistent engagement across multiple apps and devices to function effectively.
To get the most value from the system, users must maintain Apple Watch (or other wearable) usage, regularly update nutrition logs, complete mood reflections, track symptoms, and log medications.
This level of commitment may be overwhelming for many patients, particularly those dealing with chronic fatigue or cognitive difficulties. The complexity could create a paradox where the sickest patients who might benefit most are least able to maintain the consistent data input required for the system to work effectively.
-
Constant monitoring and prediction of health outcomes could transform daily life into a perpetual medical experience, potentially increasing health anxiety and reducing quality of life.
The app's alerts about symptom probability might create anticipatory anxiety that actually triggers stress-related symptoms.
Additionally, patients might become overly dependent on the app's predictions, losing confidence in their own bodily awareness and intuition.
The focus on optimisation and control could reduce patient’s acceptance of their conditions and the adaptive coping strategies that are often crucial for managing chronic conditions successfully.
4 Behavioural Science Principles
Based on the research insights and patient scenarios explored in this project, here are four key behavioural science principles that would underpin the development of an enhanced medication and symptom tracking tool:
-
Principle: People develop confidence in managing their health when they can see clear connections between their actions and outcomes, creating what Antony Bandura terms "mastery experiences."
Application in Health Tracking: The enhanced app should provide visual feedback that helps patients like Sarah connect their medication adherence and lifestyle choices with symptom patterns. When patients can see that consistent magnesium intake correlates with fewer muscle spasms, or that proactive ibuprofen use prevents severe joint pain, it reinforces their belief that they can successfully influence their condition outcomes.
-
Principle: Complex tracking systems overwhelm users' cognitive capacity, but when data collection becomes automated through habit formation and technological assistance, adherence improves dramatically.
Research Evidence: Studies show that "the probability of routine self-tracking is higher for those who use technological tools" and "the use of technological tools such as websites and tracking apps facilitates this practice." Conversely, when patients "rely on memory to do self-tracking, the chance that they will collect data routinely is significantly decreased."
-
Principle: People achieve better health outcomes when they can identify specific environmental or internal triggers and plan responses in advance through Gollwitzer's "if-then" planning framework.
Application in Chronic Disease: The research highlighted that patients need to understand "what triggers a flare up or pain" to move from reactive to proactive management. By enabling patients to track symptoms alongside environmental factors (weather, stress, activity levels), the app can surface personal trigger patterns and help users develop specific prevention strategies.
-
Principle: Patients engage more consistently with health management when they feel empowered as active partners rather than passive recipients of care, shifting from external regulation to intrinsic motivation.
Research Support: RTHM's methodology recognises that systematic tracking helps patients "regain some of their power" in managing their condition. This aligns with Self-Determination Theory's emphasis on autonomy as a fundamental driver of sustained behaviour change.